Psssst – the Zus team is heading to HLTH 2023! If you want to chat all things data and interoperability, grab time with us here.
Why is data important for value-based care?
Our first post in this series focused on defining value-based care and introducing some of the models that have since been implemented. Value-based care aims to address some of the most pressing problems in our healthcare system, such as ballooning costs and poor long-term outcomes, and to achieve these goals, organizations enabling VBC have to contend with a unique set of challenges. Unlike fee-for-service models, VBC requires the reporting and tracking of patient outcomes much more carefully both to provide better care and to get properly reimbursed. Here, we will take a brief look at some of the common VBC metrics requiring high volumes of data and how that data translates into clinical and financial success.
HEDIS Quality Measures
Healthcare Effectiveness Data and Information Set, or HEDIS, is one of the most-used healthcare quality metrics tools – as of 2016, over 90% of health payers used HEDIS to assess and collect data on the performance of their providers. Specifically, HEDIS includes a set of 92 measures across multiple dimensions with the ultimate goal of standardizing performance measures. These measures were created by the NCQA, a nonprofit organization that partners with CMS to address issues surrounding quality of care. Since then, HEDIS measures have become central to the evaluation of VBC organizations by both the government and commercial plans, and have been widely adopted as a way for payers to gauge successful outcomes.
HEDIS focuses largely on measuring clinical outcomes, with particular emphasis on preventative care and chronic care management with conditions like behavioral health, diabetes, and cardiovascular care. HEDIS ratings are used in a variety of broader evaluation metrics, such as the NCQA’s annual health plan ratings, and physicians and health systems that score well can use high ratings to negotiate more favorable relationships with payers and other partners. To be eligible for an NCQA health plan rating, plans must have scorable rates across more than 50% of all measures, and they typically pass down similar requirements to their contracted providers.
Health systems and provider organizations today spend a high volume of resources tracking and reporting on these metrics, primarily because the required data often lives in multiple systems of record that need to be manually combined; and in many cases, healthcare organizations miss out on reporting this data because it was recorded by providers outside of their system. Emerging solutions like Zus Health are solving these problems for providers by intelligently combining both internal and external data, and identifying open care gaps and missed diagnoses.
You can find a full list of all current HEDIS measures here.
Using Zus: Transitions of Care
It’s no secret that we at Zus love healthcare data, and we also think we’re pretty good at making it usable for a variety of provider needs. One of those needs happens to be boosting HEDIS performance, especially in the Effectiveness of Care category. For example, HEDIS evaluates metrics related to transitions of care for Medicare patients, with the goal of incentivizing healthcare providers to proactively engage with their patients after an inpatient admission. To date, health plans have had low results (<25% patients meeting the criteria) for two specific measures:
- Notification of Inpatient Admission. Documentation in the medical record of receipt of notification of inpatient admission.
- Receipt of Discharge Information. Documentation in the medical record of receipt of discharge information.
The overall percentage of patients meeting these measures across Medicare HMO and PPO plans is below:
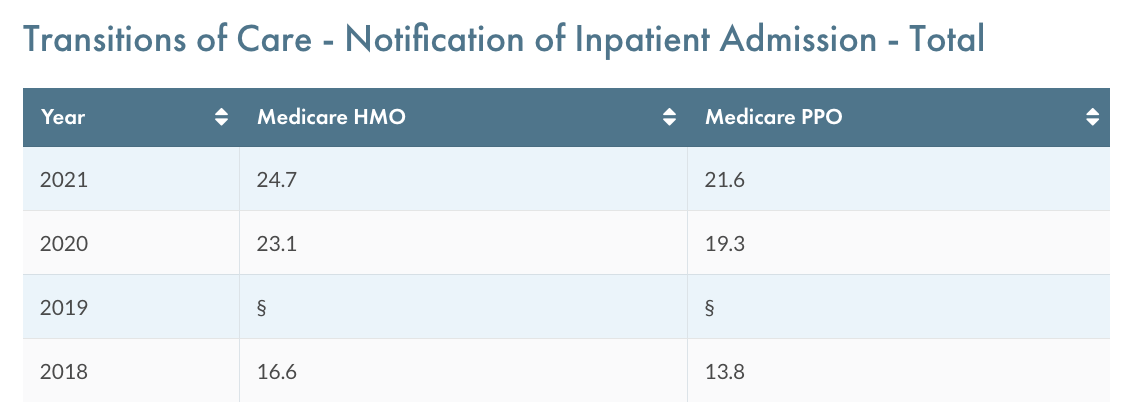
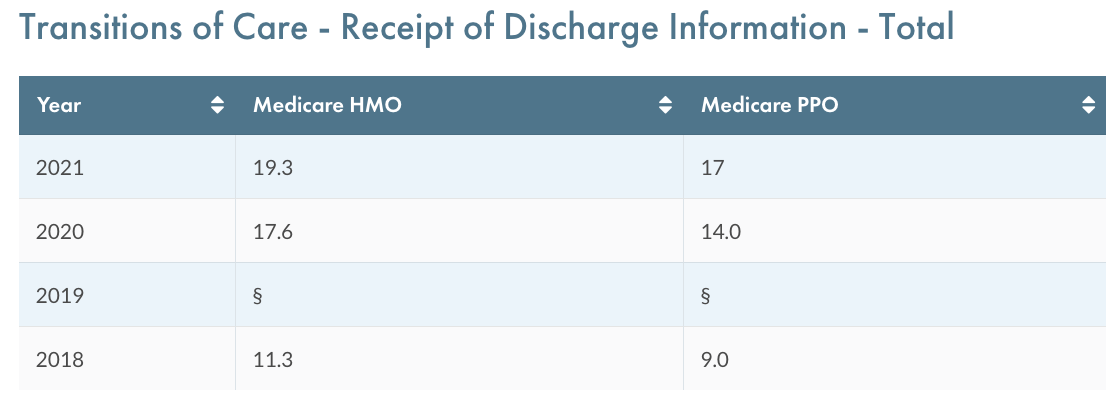
There are a variety of potential reasons for these low results: in some cases, providers may not be receiving the notification or discharge information because of lack of connectivity to external systems. In others, they may be receiving this information but not properly documenting it in the medical record, in a way that can then be used by the data analysts creating HEDIS reports.
Luckily, the Zus Aggregated Profile can help with both of these needs (and more!). Our ADT (Admit, Discharge, Transfer) solution is designed to ensure providers never miss another notification of inpatient admission. With connections to hospitals covering over 200 million patients across the country, Zus users receive real-time alerts when their patients are admitted to the hospital, and can choose from a variety of ways to receive these alerts directly in their workflows. Current customers have opted to receive ADT alerts via API, Slack notifications, and more. To make it even easier, Zus has bidirectional connections with multiple EHRs so that no extra work is required to document the inpatient admission in the medical record.
On top of all this, Zus goes the extra mile by standardizing all of this inbound data and making it available in our customers’ data tool of choice via the Zus Data Mart. If the data exists, we want you to be able to access, use, and report on it as easily as possible, which comes in especially handy for HEDIS metrics. While the national average for the HEDIS Notification of Inpatient Admission metric is 22 – 25%, Zus’s data solution can help providers meaningfully boost their performance with our coverage of over 60% of patients across the country.
Zus also has a unique refresh engine that automatically searches for related data points across our networks based on recent patient information that we’ve received. This is particularly helpful for the Receipt of Discharge Information metric. Whenever Zus receives an ADT alert for a patient, our refresh engine automatically searches for a discharge summary document from the admitting hospital and makes it available via Zus if one exists. Instead of asking staff to spend time calling the hospital, getting routed through a phone tree, and waiting for documents to be faxed, providers using Zus can access these discharge summaries with minimal effort and improve performance on this important HEDIS metric.
Because HEDIS metrics are widely adopted, they are frequently used by purchasers to make comparisons across health plans, and by these health plans to evaluate the performance of their contracted providers. Performing well across the broad list of metrics has never been more important, and if you think Zus can help, be sure to get in touch.
Featured photo by Neil Thomas on Unsplash