This may sound odd coming from someone like me who has long worked in healthcare technology, and especially as the literal co-founder of an EMR company, but in the same way that we saw paper patient records heading toward extinction decades back, the EMR as we know it is beginning to wobble. It’s like an aging boxer in round 13 taking on a younger, faster opponent.
The word EMR is a noun, a static thing. In truth, when we use the term, we far more often have an active idea in our minds, making it more like a verb. And in fact, many paragraphs and entire books are dedicated to describing and understanding what an EMR actually is. The U.S. Government has gotten in on the act, with a corpus of literature, revisions, artifacts, checklists, commentary, and guides — all to define this one thing.
So I ask you: What is an EMR?
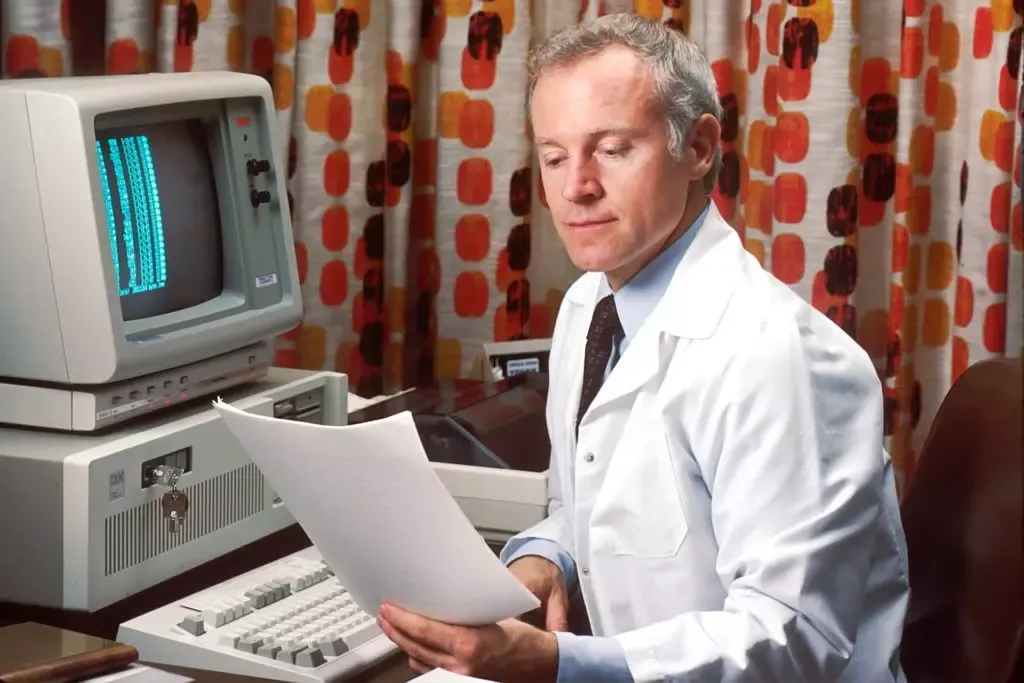
It’s easy to hearken back to the pre-digital era and remember the patient chart, stored in a filing cabinet in our doctor’s office. Its simplicity and the simplicity of that analog era may seem quaint, but it was easy then to define a medical record. It was one individual doctor’s record of what had been seen and done with their own eyes and hands for a given patient.
The promise of the electronic era was romantic and ambitious — to break down the silos of a world before computers and build a composite, complete picture of the core clinical information about a patient. It would encompass the work of many hands and eyes of all the doctors who touch a patient — untethered from geographical boundaries.
But that’s not what’s happened. Instead (and unsurprisingly) form has followed function. EMRs became mechanical turks for the original myopic recordkeeping of the doctors of yesteryear. Only this time, to pay for their added time and expense, they were way “more so.” EMRs enabled documentation far more than a doctor’s hand would ever bother to capture (thus making the billing codes a little higher). Anything the hands and eyes of a doctor did to that original paper chart was fully captured in highly compliant and extremely legal bloat-script. And to do that, EMRs included lots of other things we somehow added to their original definition. Like a deranged and perhaps half-blind baker, we threw together a recipe — a pinch of front-end workflow, a dash of software processing, and of course a handful of storage capabilities. We mixed it together haphazardly, and then we required it universally.
I think of today’s EMR as a three-layer cake.
Layer one: The Workflow. You know the drill: Check-in (“insurance card please”), intake (“Smoker?”, “How many packs?”, “Can you step onto this scale?”), exam (“Cough please”), orders (drugs, labs), check-out (“that’ll be $95 and please take a card to schedule your radiology from the stack in the sliding window”). These are the step-by-step tasks that the EMR software walks staff and providers through in order to produce a consistently-documented and compliant encounter, one that does not lend itself to lawsuits but is as billable as possible.
Layer two: The Compute. The data captured through those workflows in the first layer is then used to gonkulate new info. CPT codes are calculated and defended by ICD codes, interview data, and time logs. “Meaningful Use” metrics are calculated and attested to, for quality, of course, and of course also for other payments. Quality scores are gonkulated again as referral forms and automated “consult letters”. Tremendous amounts of compute are funneled single-mindedly to turn the clinical experience into financial outcomes, whether fee-for-service or “value-based” care.
Finally, layer three: The Storage. Unfortunately, this is not the storage we might want, a longitudinal profile of the patient with relevant aspects updated frequently. Instead, it is the storage of all of the above metrics generated by the compute, geared simply to be ready for audits and questions. Armed with this storage, providers hope desperately not to be embarrassed when patients come back expecting to be remembered. This has led to many EMR cartoons that feature blind men and elephants, as even the most wizened experts struggle to adequately identify what EMR they are looking at.
All this has contributed to an enormous explosion of healthcare vertical monopolies (and related price increases) across the country. Many have rationalized that if an EMR is only to be a “core sample” of the Workflow, Compute, and Storage of one physician’s experience, then the logical thing to do is to move all the physicians a patient sees under the same EMR roof. Such consolidation has created a mirage of “continuity of care”.
As EMRs have matured and regulators have blanched at the silos created by their original mandates and incentive programs a decade ago, the ecosystem has slowly nudged itself towards sharing. Record sharing (originally mandated by HIPAA) is becoming a norm, with common sharing services like Commonwell yielding a 20% match rate for Epic record queries and a 70% match rate for Athenahealth (the company I founded). It’s increasingly common now, as a doctor looks at their patients, for them to find externally-generated data in a patient’s EMR. Such a record is not machine-readable, allows no alerts to fire on that data, and leads to few algorithmically derived insights. But it’s a helluva lot more than nothing, even as it’s a helluva a lot less than we deserve.
My summary is that EMRs are OK as they are today, but absolutely nothing compared to what they could, should, and maybe will be in the very near future.
So what should EMR mean? Let’s go back to those three aspects: Workflow, Compute, and Storage.
First, we need to liberate that Workflow layer which today means a thousand things. Most of the workflows are unrelated to moving people through old-school office visits. In old EMR speak, we called this concept “the encounter,” and it was tied tightly and rigidly to care delivered over an exam table or hospital bed.
The new workflows are different. They are the always-on, often nearly free, constant contacts of the digital health age. Think of such workflows as the “edge computing of care”. K Health and Buoy Health will give you free bot-doctoring that is getting better and better. And a dozen more digital health players will give you weirdly-affordable super-fast online team-based care.
The new explosion of health communication means text threads, care plan alerts, and group messaging, which offer ongoing relationships and community with providers and with patients like you. These workflows will be more important than office visit workflows going forward. The original workflow engines, so a long part of traditional EMRs, should also be able to write to our records. But so should thousands of additional applications and sources.
All of this demands a totally different workflow engine. What about passive monitoring of exercise, or steps, or glucose levels? There are whole companies yet to be built that are centered on new care modalities that have nothing to do with exam rooms.
Now let’s relook at Compute. Sure, we should be able to compute codes and bill them. Why, though, are we stuck with EMR’s Compute being entirely geared towards claims? New age providers are increasingly creating products that don’t fit neatly within the world of the CPT code. Many are asking for a monthly subscription fee from employers and payers. Then those organizations purchase pieces of their care product that they don’t provide with their own staff, not unlike a general contractor with subcontractors.
New age providers will need to buy care as often as they bill for it. Where is the Compute to direct that spend? Where are the ledgers? Back in the third party administrator days in California, there were a few rudimentary capitation management apps, but they are ancient and not connected to anything. Firefly Health, the company where I serve as executive chairman, bills employers for its care but also pays specialists for jumping in on sticky cases, which eliminates the need for a full-on referral.
There is also a whole category of marvelous Compute that will come as we more routinely ingest social-determinants-of-health data, which is super important. The dominant providers and their fee-for-service (FFS) agreements are technically interested in such things, but cannot make such things core to their systems and processes. There is not enough return to FFS-dependent providers to incentivize their radically reducing fees generated by patients.
Other Compute could surveil populations for what’s working and what’s not, for the purposes of making real-time trade outs. Again that’s not a thing traditional FFS business models can afford to care about, but will be a major win for all new age, value-based players. As more and more healthcare players are born digitally native, there will be more and more APIs to call to calculate care coordination. For example, can you schedule across all the siloed electronic calendars in medicine today? Looking outside healthcare, Kayak has no problem interacting with all the calendars of airlines worldwide. Such discrepancies point to a dramatic misappropriation of where we currently spend our industry’s Compute.
Finally, Storage. What should we store? Core samples? Blind man soundings? Of course not. The term EMR should refer to the record and only the record — a complete operational data store for every American. Meanwhile, digital health companies today are intentionally narrow. Ria Health, for example, makes no bones doing anything other than alcohol treatment. They have no plans to do a middling job at X-rays and colonoscopies and all the other things traditional IDNs seek to cobble together. They plan to do alcohol treatment well and, to do so, they need to get a really complete, comprehensive and continuous view of their subjects.
We should all have an EMR, and it should operate like our LinkedIn profile — when we make a change to it, everyone following us should be able to know right away. There can be no “Save as PDF” and re-sending to friends and prospects. This is what digital-native companies must have. Such companies have no interest in guarding their evidence of care on a patient. In fact, they know they do a much better job when their understanding of members is complete. In that way, they are natively sharers, for both selfish and inherently good reasons.
In my old EMR life, we talked about the scalability of technology. Today, “extensibility” is just as important. Can a tech-native provider build its own workflows and have them seamlessly co-exist with “rented” ones? Can they do the same with their compute? And of course, as with Spotify, can they dispense with keeping an out-of-date, memory-hogging copy of just their own songs alone and instead get a database of all the songs in the world? We know how to do this shit. In fact, in parts of our lives that we care about much less deeply, we do it all the time.
Simply put, the EMR we have come to know does a very important thing. But god willing, we will need it less and less. EMRs grew up to do a certain job, at a certain time, in a certain place. They are not wrong or bad, but they are closely related to the rapidly-diminishing office-based, fee-for-service world. As digital health companies move from being cool parlor tricks and gadgetry to the mainstream, let’s hope that “place” moves into the rearview mirror.
This piece also appeared in Techonomy on December 3, 2021.