In our last Pipe Dreams post, we unpacked the limitations of surface-level interoperability—data pipelines that deliver information, but still leave care teams buried in PDFs and portals with no clear next step. Today, we’re focusing on one of the noisiest signals in healthcare: the ADT alert.
First, ADT stands for Admit, Discharge, and Transfer—event-based notifications that signal when a patient has had an encounter and track the movement and status of patients in a healthcare facility.
In theory, ADTs are foundational to care coordination. In reality? They’re more like an overactive smoke alarm—blaring without context, leaving care teams scrambling for critical details. Instead of providing a clear clinical story, they flood teams with alerts that only leave a breadcrumb trail to follow.
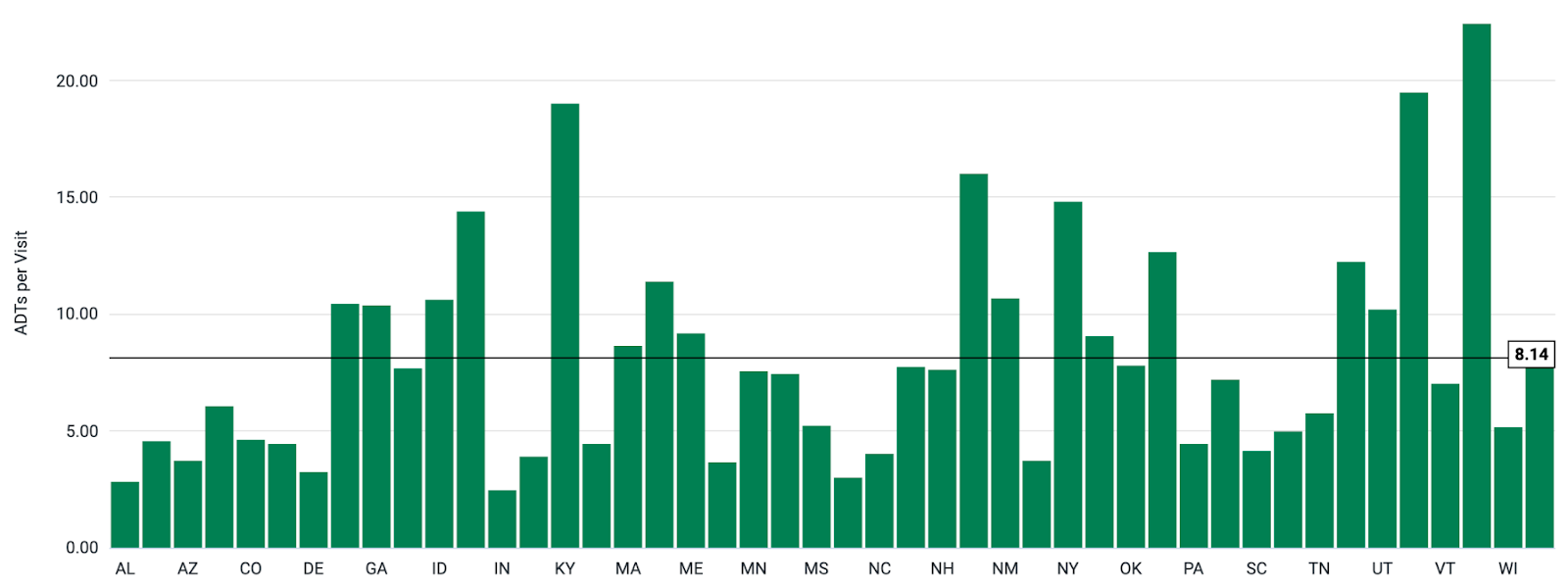
Here’s the real world breakdown we see from our networks. Patients are generating an average of 8.14 ADT messages per encounter, creating more noise and work for care coordinators to sift through.
Why Transitions of Care Matter (Especially in Value-Based Care)
In value-based care (VBC) payment models, providers get rewarded for outcomes, not volume. This means that providers must step in before the next avoidable admission or costly duplicate test. Strong transitions bridge the gap, preventing avoidable admissions and reducing costs.
Transitions of care have three core benefits:
- Reduces Readmissions: Prevents penalties from programs like the Hospital Readmissions Reduction Program (HRRP), and preserves reimbursements.
- Improves Quality Metrics: Boosts scores like Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) by ensuring timely, informed follow-up. This can increase bonuses and incentive payments.
- Enhances Care Coordination: Eliminates unnecessary services, lowering costs AND improving outcomes.
Flashback to our last Pipe Dreams blog. Interoperability can feel like alphabet soup. Download our cheat sheet designed just for you.
Real-Life ADT Overload: A Common Scenario
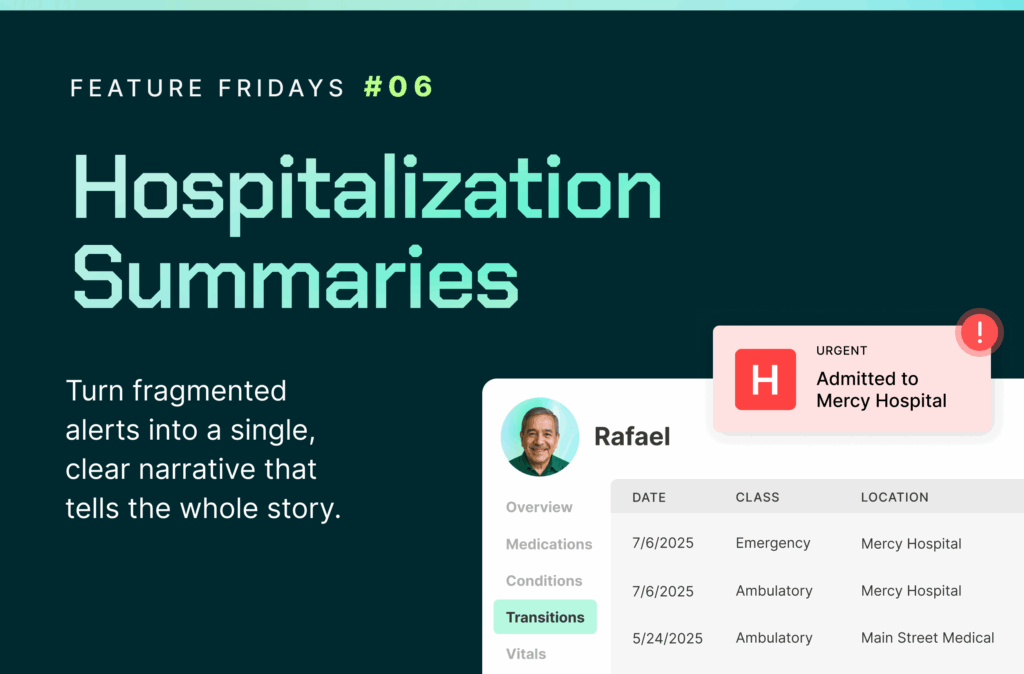
Say a patient visits urgent care for shortness of breath, gets transferred to the ED, evaluated, given medication, and discharged with a new care plan.
As a care coordinator I need to know about this whole series of events to ensure the appropriate follow-up care is delivered and readmission is avoided. This means adjusting the care plan, coordinating with a primary care doctor, and assessing whether medication needs to be adjusted.
But here’s what the care team might see:
- A01: Urgent Care Admission
- A04: Registration
- A08: Info update
- A03: Urgent Care Discharge
- A01: ED Admission
- A04: ED Registration
- A02: Internal ED Transfer
- A03: Final Discharge
This is 8+ messages, most without meaningful clinical context. Care coordinators must sift through these to figure out what actually happened and if follow-up is needed. If needed, they will have to call the hospital for discharge summaries or additional documentation, spend hours sifting through various file formats and making phone calls and faxes, to finally engage the patient and effectively coordinate next steps.
This is the reality for most teams: a stream of alerts dumped into inboxes, fax machines, or ignored portals. Each one a puzzle piece with no image on the box.
Even worse, many vendors stop here. No grouping. No filtering. No documentation. Some may retrieve a discharge summary after an ADT ping–and they may even deliver it in seconds–but speed doesn’t equal clarity. Without marrying all the related discharge summary to the fully deduplicated transition of care, it’s just more noise and another isolated alert with no clear action.
From Static Alerts to Actionable Episodes
Here’s how forward-thinking care orgs are improving transitions of care:
- Pull encounter data from multiple sources: Don’t rely on one feed. Pull from ADT, national networks and HIE to avoid missing events.
- Group Alerts into Episodes: Don’t rely on one feed. Pull from ADT, HIE, and national networks. Collapse alerts into unified episodes of care.
- Add Context: Pair alerts with discharge summaries, medication lists, and care plans.
- Deliver at the Right Moment: Summarize alerts to show up when they matter, in the right system of use.
- Follow Up with Confidence: Know what happened and what to do next so you can help the patient in their care journey.
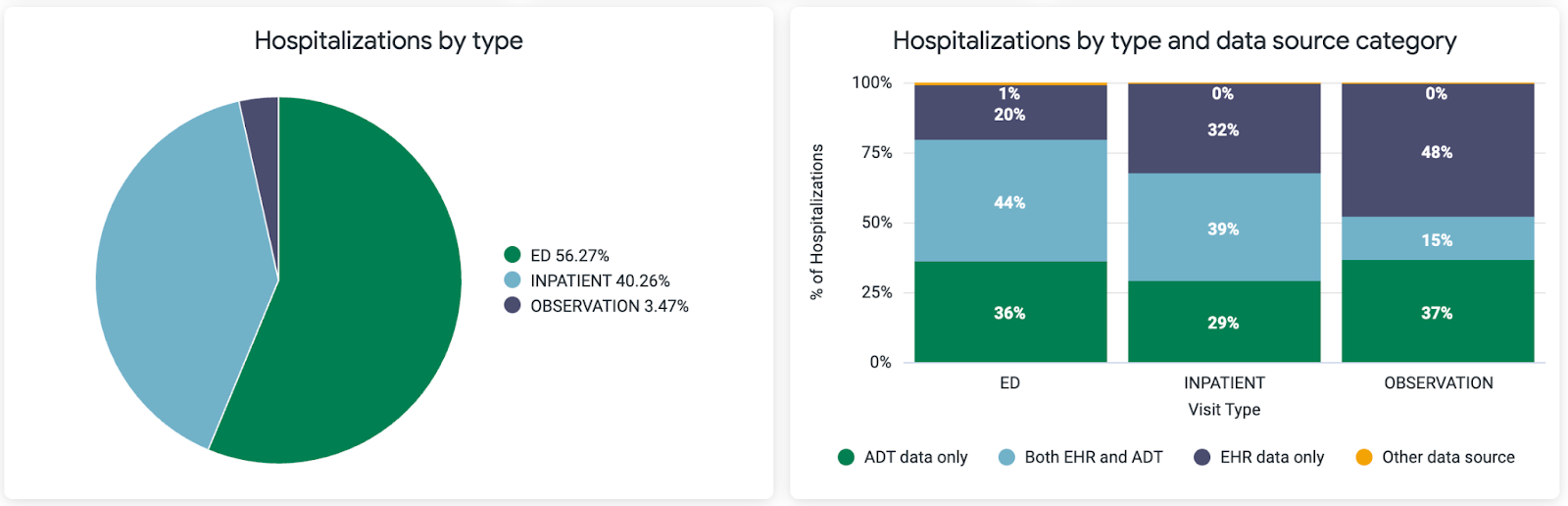
If you rely solely on EHR networks or ADT networks to track hospitalizations, you’re likely missing up to 50% of the story. ADT alerts provide thin HL7 messages, missing clinical context. On the other hand, EHR networks pull data later, so you miss out on real-time updates. This is true of any encounter whether it is Emergency, Inpatient or Outpatient.
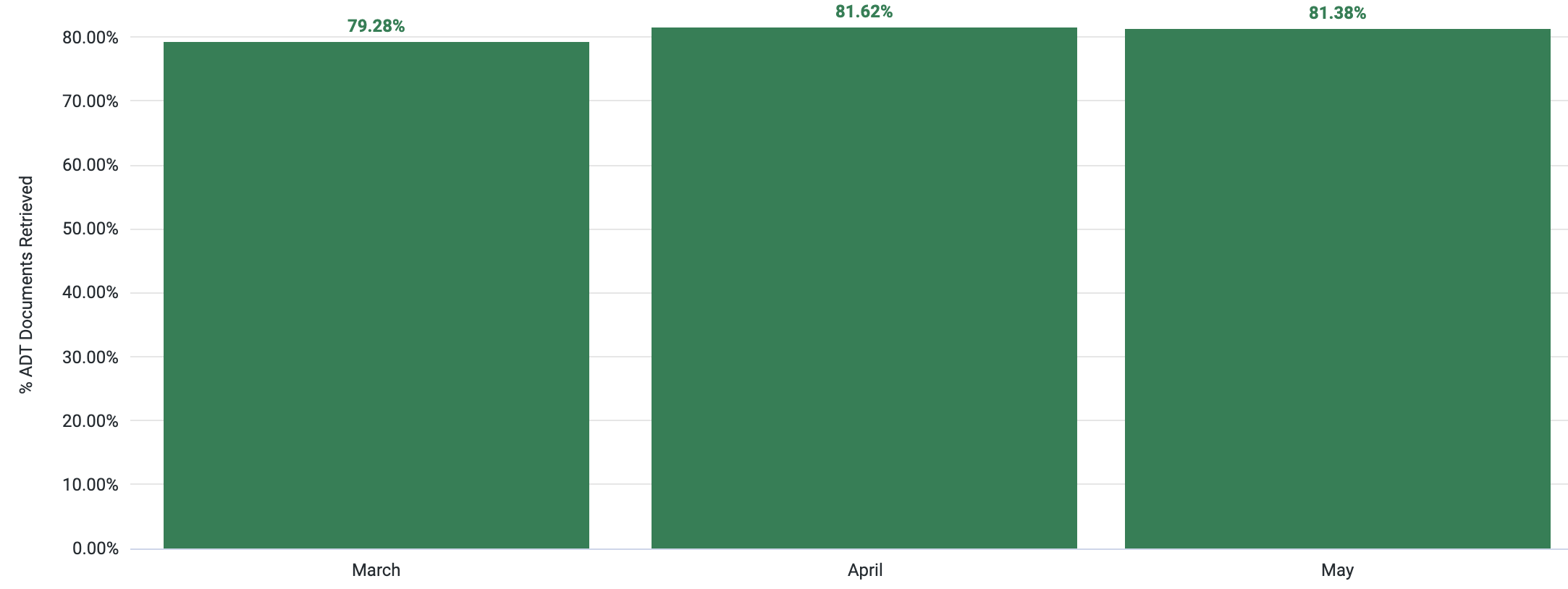
Relying solely on ADT data gives you a real-time alert that an encounter has occurred, but offers little clinical detail to guide next steps. On the other hand, querying EHR networks provides the clinical context care teams need, but often comes too late—because without a timely signal, you don’t know when to request that information. By combining both ADT and EHR data, Zus bridges this gap: care teams are notified quickly when a patient has an encounter and can immediately seek the relevant clinical documentation. As a result, corresponding clinical documentation is automatically retrieved 80% of the time. This approach saves hours by replacing the reactive scramble for information—chasing faxes, logging into multiple portals, or searching for missing files—with proactive, coordinated care.
We also pull in multiple ADT alerts per patient, then clean things up by grouping them into episodes of care. Think: one coherent story instead of eight scattered messages.
Still, grouping alerts is just the beginning. On their own, raw alerts still don’t tell you what actually happened. That’s why Zus goes further, pairing those alerts with the clinical narrative—discharge summaries, medication lists, care plans—using nationwide networks like Carequality, CommonWell, and the new QHIN framework.
Some vendors and approaches stop short here, pulling a discharge summary as soon as an alert is fired. But a single document doesn’t tell the full story. Without tying it back to the broader episode of care, it’s just another disconnected data point that care teams must sift through and add logic to.
And because patients are seen at facilities irrespective of EHR vendor, the nationwide networks are the perfect vehicle to pull those encounter summaries from.
This means more follow-up appointments happen. More patients stay on track. And fewer wind up back in the hospital.
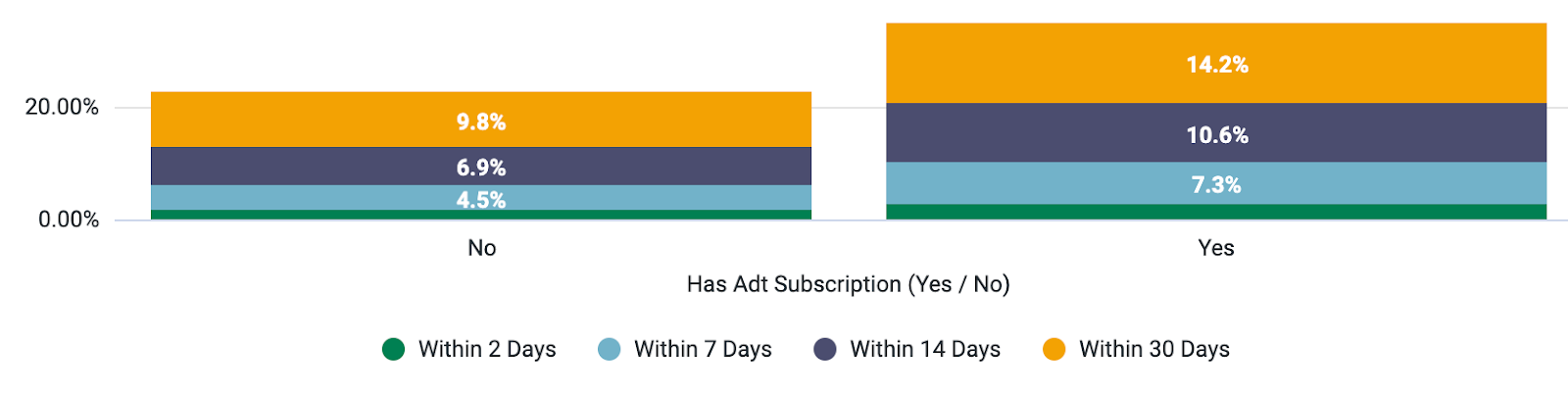
And the results speak for themselves. Our customers see a 64.2% increase in patients booking and showing up for appointments after an event within 30 days post discharge.
From Noise to Impact:
With Zus, care teams can:
- See 33% more hospitalizations that would otherwise be missed by relying on ADT feeds alone.
- Save 90 minutes per day by grouping alerts into episodes of care (8:1 average alerts grouped per episode).
- Access EHR documentation for 76% of transitions of care.
These aren’t abstract improvements—they translate into real operational wins. In fact, one of our customers saved enough time to handle 120 more patients per month without adding staff.
Wrapping Up
Turning noisy alerts into meaningful transitions isn’t just a workflow improvement. It’s a strategic advantage in value-based care. When you combine signal detection with rich documentation and smart delivery, you empower care teams to act, not react. Care teams are set up to intervene earlier, follow up more often, and close more gaps that actually matter.
Because transitions of care shouldn’t feel like guesswork. They should be the moment everything comes into focus.
Up next in Pipe Dreams: Patient engagement. We’ll explore how better contact information and smarter outreach signals—like recent hospitalizations or newly identified chronic conditions—can dramatically improve patient connection rates, especially for hard-to-reach populations. Because the first step to better care is reaching the person who needs it.