
This is the first post in our Pipe Dreams series — lessons, tips, and real-world guidance for building smarter healthcare data networks. Throughout the year, we’ll share what we’re learning on the front lines of interoperability to help you go from raw data, to clear insights, to better outcomes.
Healthcare is in the middle of a seismic shift in how data moves. With TEFCA rollout accelerating, QHINs going live, and more providers leaning into value-based care models, the ability to access and act on clean, comprehensive data isn’t a “nice to have” anymore, it’s a competitive advantage.
For digital health teams, the stakes are high. Without the right data at the right time, you risk data overload, missed care gaps, and wasted outreach. How you manage data flow can determine your success.
Healthcare Interoperability: Learning the Language
Let’s start with the basics – acronyms! TEFCA. QHINs. HIEs. FHIR. EHR APIs. And if you don’t speak ‘interoperability,’ it can feel like everyone else is having a conversation you’re not part of.
Here are a few core terms:
- TEFCA – the national framework for health data sharing
- QHIN – the new highways for interoperability
- FHIR – the modern data format driving APIs
- EHR API, HIE, ICD-10…and more.
These terms are the foundations of interoperability: the vocabulary and infrastructure that make data exchange possible.
Want to go deeper? Our Interoperability Cheat Sheet breaks down the full list of acronyms—plus strategies, pitfalls to avoid, and tips for turning data into action.
Download the cheat sheet built for digital health teams.
The Real Challenge with Healthcare Data: Connections Alone Aren’t Enough
There’s a common myth in healthcare data: once you have the right connections in place, your data problems are solved.
Not so fast my friend.
Healthcare data is everywhere. TEFCA. QHINs. HIEs. EHR APIs. (See alphabet soup above.) But before you can make use of it, you need to know what to look for — and where to find it.
That’s why smart operators think in terms of both finding the right data (breadth and depth) and making it usable (organization, summarization, workflow and real-time delivery). Because finding data is actually easy once you know where to look and there are a plethora of vendors out there who can retrieve data. Making it valuable is a whole other story.
That’s where platforms like Zus focus. It is not just about pulling data from everywhere, like national networks, local HIEs, and your own systems. It’s about transforming it, normalizing it, deduplicating it and enriching it. And ultimately making it usable by the people who need it most: care teams, in the systems and workflows they already use every day.
Breadth: How Wide is Your Coverage?
Think of breadth like surface area: the more places you’re connected, the higher your odds of knowing something about your patient.
National clinical networks like Carequality, CommonWell, and the QHINs provide broad clinical coverage for patients, while regional networks like HIEs offer richer, more localized data. Medication data is best sourced from pharmacy networks like Surescripts, while lab data mainly traces back to Quest and Labcorp.
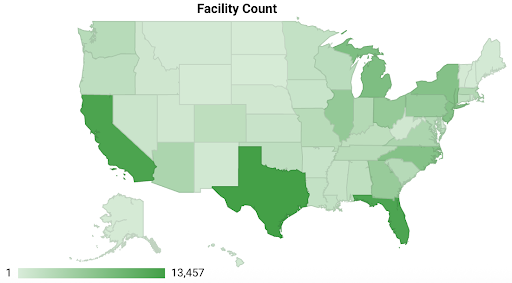
These national networks compromise over 100,000 facilities across the country and cover in excess of 300M lives.
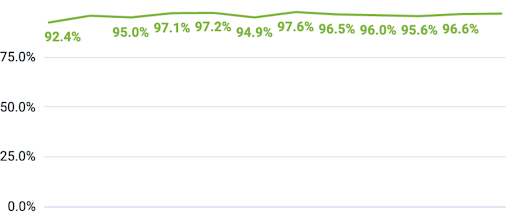
A quality implementer on the network should be expecting matching likelihood for patients in the 80th+ percentiles, depending on the composition of the cohort.
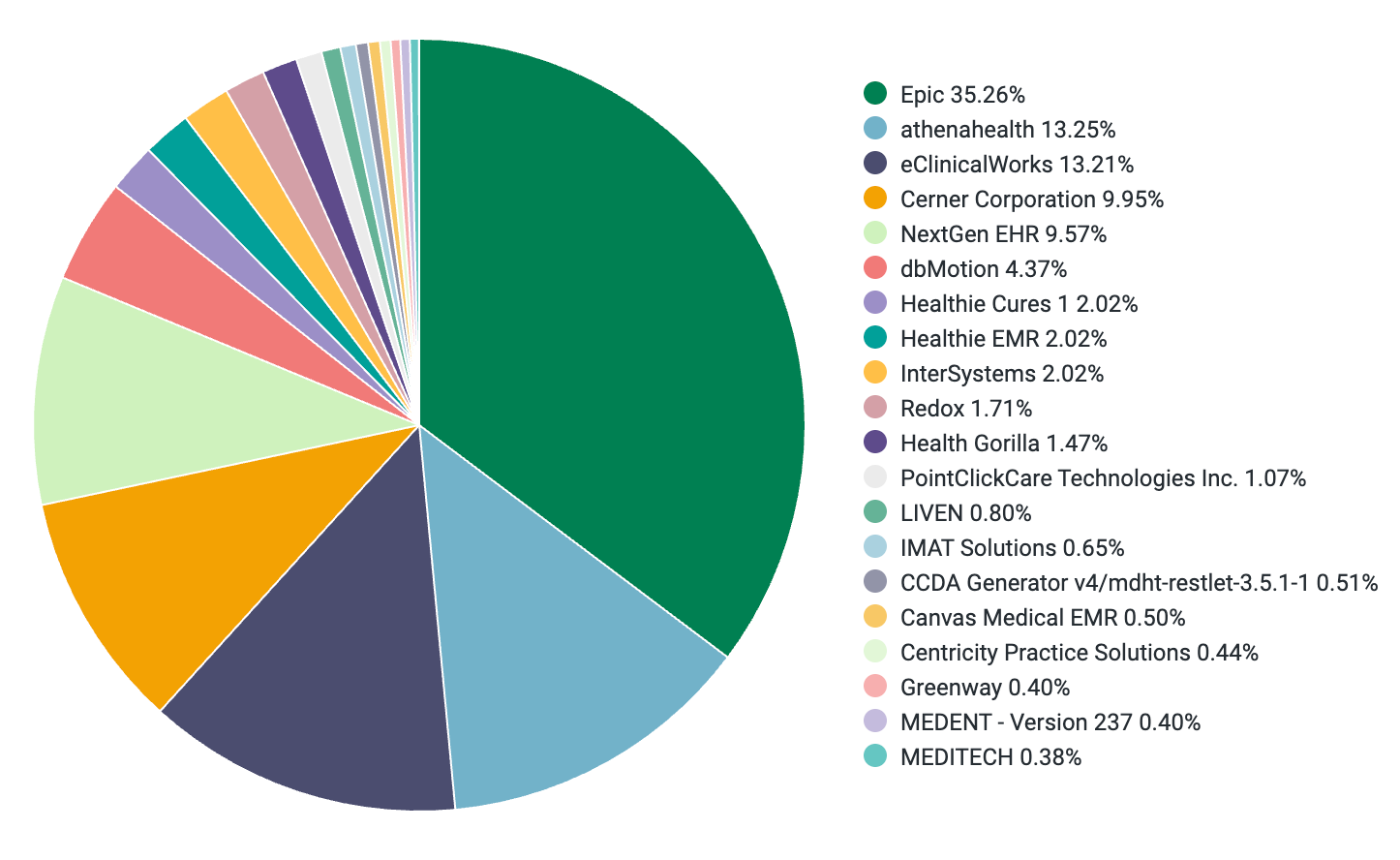
Coverage isn’t just about geography. It’s also about system compatibility. Zus connects across all major EHR systems certified by ONC, ensuring we meet patients (and their data), where they actually receive care.
The smartest data strategies don’t pick one. They stack them. Breadth gets you coverage and a signal. Depth provides richness and context to work with.
Depth: How Detailed is Your Data?
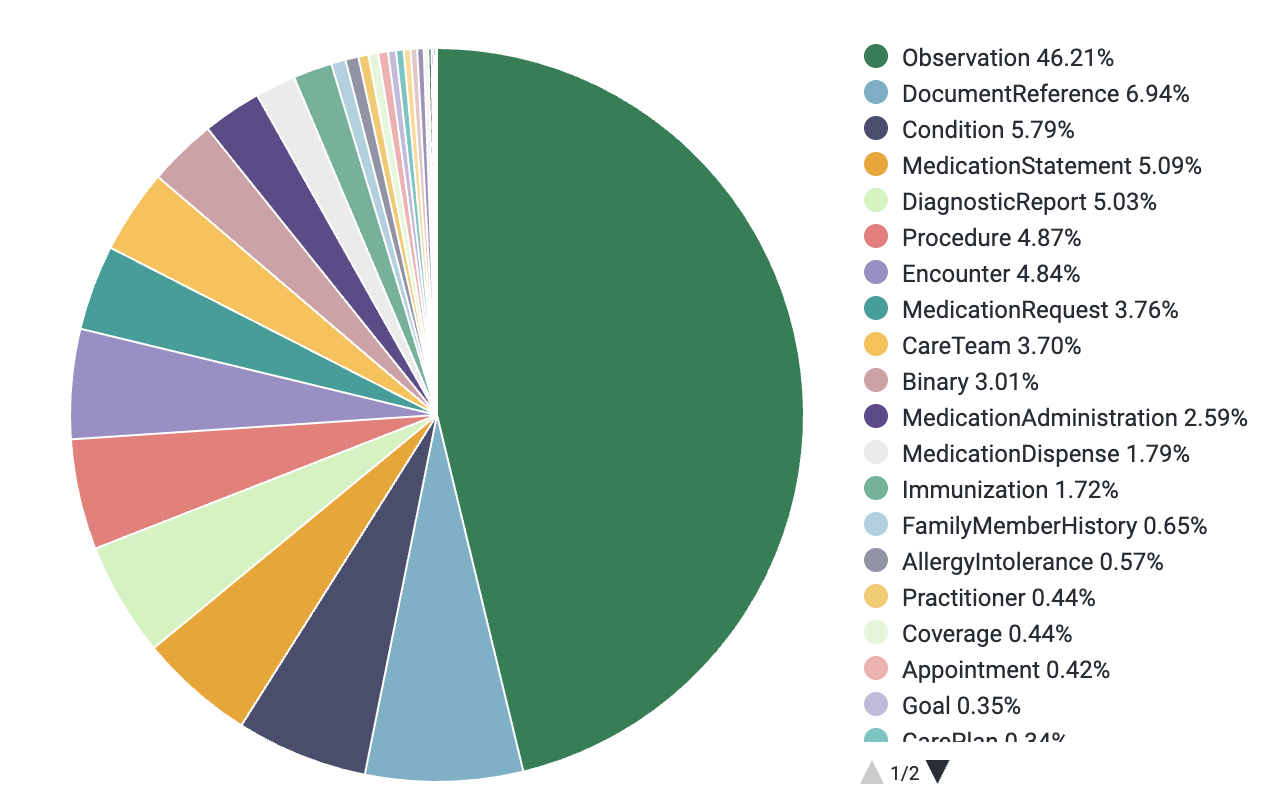
At Zus, every time we pull records from the clinical national networks, we get about 200 documents per patient. We map that to over 1,000 raw FHIR resources.
Here’s a real sampling of documents Zus pulls per patient and subsequent FHIR resources mapped from them.
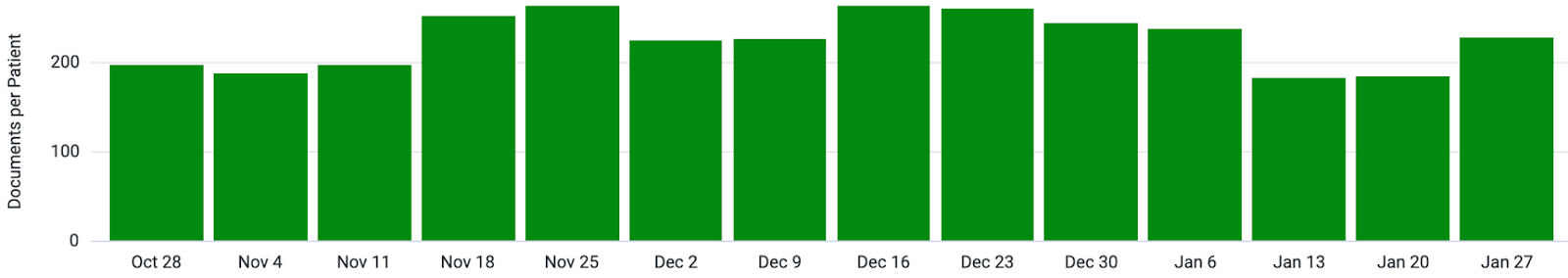
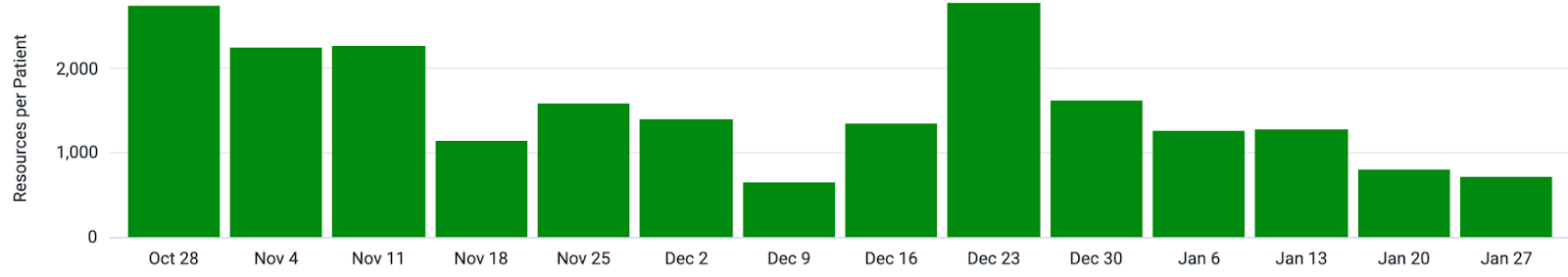
That’s a lot of data for just one patient, but it’s not yet information. In fact the simple act of pulling this data from Commonwell, Carequality, QHINs is a commodity, what comes next is where the real value lies.
Without normalization, deduplication, enrichment and summarization, that volume becomes noise. Turning data into actionable insights is what makes it valuable.
Volume isn’t the problem. Meaning is.
Push data is when information comes to you automatically as a notification that something important just happened. Event Notification Services (ENS) send real-time alerts when key events happen, like when a patient gets admitted, discharged, or transferred (ADT events). These are critical for care teams managing active patient populations or programs that require quick intervention, like emergency departments or medication adherence programs.
But push data is far from perfect. ADT alerts are noisy, incomplete, and missing key context. More often than not, a notification is just the start — care teams still have to follow up, make calls, and chase down the full story. Look for solutions that can separate the signal from the noise and deliver clean actionable alerts.
Depending on whether you’re pushing or pulling, timing can be everything. That’s why smart operators combine both.
And that’s exactly how Zus works. In addition to pulling data from national and local networks, we layer in always-on querying logic that watches for signals – like a new hospitalization or incomplete medication refill – and automatically initiates targeted queries to create alerts and fill in the gaps. No manual chasing. No guesswork. Just timely, relevant updates delivered into workflows care teams already use.
It’s how our customers know things like:
- A patient hasn’t picked up their medication refill
- A patient has shown up in an ER, and they receive an alert, with consolidated notes in hours
- A patient has a specialist appointment that was scheduled outside their network
Because it’s not just about combining push + pull intelligently. Look for solutions that allow you to subscribe patients that automatically keep patient records updated by combining both methodologies.
Final Thought
If you want better outcomes, better care, and better patient relationships — you need more than just pipes.
You need bridges.
Bridges between data and action. Between signals and strategy. Between knowing and doing.
This is what we’re building at Zus. And in our next post, we’ll show how those bridges come to life during transitions of care. I’ll break down how to combine ADT alerts with targeted queries across Carequality and CommonWell to give care teams a real-time, reliable picture of what just happened with their patient and what to do next. Because knowing a patient was admitted or discharged is one thing. Acting on it fast with summarized notes just a click away? That’s where outcomes change.
💡Need a quick reference for the acronyms and standards mentioned above? Download our Interoperability Cheat Sheet — a simple guide to the data standards powering healthcare today.
