In this post, Zus physician advisor Dr. John Dayton shares an example of how the Zus Aggregated Profile helped him deliver more informed care to an ED patient.
Context
I work at a critical access hospital in a small, rural community. Our hospital has an emergency department (ED), inpatient ward, and obstetric unit, but we don’t have any specialty support for orthopedics, cardiology, or neurology. As an emergency physician, I often see and stabilize patients who need to be transferred to a tertiary hospital for specialty care. I’m able to see medical records for our hospital, but our electronic health record (EHR) is unable to access treatment records for our patients when they are seen at nearby hospitals or when they are transferred several hundred miles for specialty care.
When I was working an overnight shift, I saw an 80-year-old female who presented to the ED with a chief complaint of fatigue. She spoke limited English, arrived via EMS without her family, and was unsure of her prior diagnoses or medications. This patient usually receives care at a nearby facility and had recently been admitted to a tertiary academic center over 200 miles away.
This case presentation has the traditional format with the chief complaint, workup, differential diagnosis, lab and imaging results, and disposition. I’d also like to highlight how I addressed finding information about the patient’s medical history and discuss a new resource I used.
The Patient Case
Over the last two days, this patient had become increasingly tired, noting difficulty breathing upon exertion. She lives with her family, and none of them are ill, she is a non-smoker, and she’s had both COVID-19 vaccinations and boosters. She denies fever and chills and notes that her B12 has been low in the past. In a stroke of good luck, she actually brought some medical records with her to the ED. However, the records are outdated and consist of the following:
- Patient discharge instructions after a laparoscopic cholecystectomy in 2005
- An X-ray report from a knee injury in 2013
- Lab records showing a low Vitamin B12 level from 2017
- Vaccination card from 2020
She then asks, “Do you think my B12 is just low?”
Her vital signs include the following:
- HR = 109, BP = 110/70, T = 100.0, RR = 28 satting 94% on room air
Her exam findings include:
- General: Alert and pleasant, but fatigued
- HEENT: Nares clear, no pharyngeal erythema
- Cardio: Regular rhythm with mild tachycardia
- Pulm: Tachypneic, decreased sounds diffusely, no wheezes or crackles
- Abd: NTND, no surgical findings
- MSK: No obvious trauma or leg swelling
- Skin: No cyanosis, pallor, or rash
This presentation has two treatment dilemmas:
- The first is that I need to diagnose and treat the patient
- The second is that I need to find more information about her medical history
At the very minimum, I’d like to know about her chronic and current medical problems. I would be able to get an idea of her current medical needs if I could find out what medications she had recently been prescribed and was taking. I’d also like to know about the workup and diagnosis from her recent hospital admission. This type of admission, discharge, and transfer (ADT) data would also help me understand why she had recently been admitted to the academic center and would also provide information about her medical history, hospital workup, and discharge diagnoses.

Since the patient was was showing signs of rapid, shallow breathing, our team put her on oxygen. For the patient’s medical workup, I checked basic lab work, a COVID swab, and a chest x-ray. Given concern for cardiopulmonary symptoms, I also added a troponin, and a d-dimer test to screen for pulmonary embolism (PE). In the meantime, I reached out to several resources to find the patient’s medical history, including the EMS team and the patient’s family. Because I saw this patient during a night shift, I was unable to contact her nearby clinic where she receives most of her care. When I reached out to the academic center where she had recently been admitted, I was told that I would need to call during daytime hours when medical records would be available. I found a similar situation with local pharmacies.

After the oxygen had been given via nasal cannula, the patient was more comfortable. Her lab work, imaging results, and EKG were returning as my team and I made several unsuccessful attempts to obtain more information about her medical history. Her workup was remarkable for an elevated d-dimer, and she was sent to CT for an angiogram so we could check the vessels in her lungs for PEs.

Based on her workup, I was concerned the patient had one or more PEs. If the chest CT was positive, I was thinking about what medication I’d use, especially given that selecting the best medicine would depend on her history, which I did not yet have. If she had PEs in the past, and was off medication, she’d need to restart it. If she was already being treated for PEs and had failed outpatient treatment, that would need to be factored in when choosing a stronger medication. If she’d never had a PE, this would also factor into the decision of what medication would be best to initiate.
In the meantime, I was reminded of my limited bandwidth as a trauma patient arrived to the ED with a stab wound that required stabilization. He joined the other six patients I was treating at that time.

Using Zus
I’ve been working with Zus to ensure their Zus Aggregative Profile (ZAP) has the medical history that physicians need for transitions of care and scheduled visits with their patients. We’ve been working on the best way to display information such as a comprehensive medical history, a current medication list, and recent lab work. Even though this is most often used by physicians to review patient information before a scheduled visit, some of the information (like current medications) can be populated in just a few minutes. When I looked for the ZAP on my patient, this is what I found:
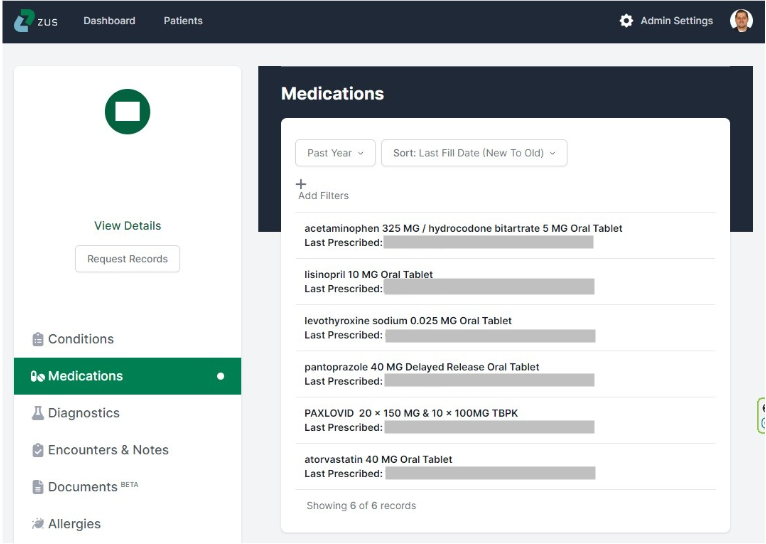
In just a few minutes, I was able to find prescription info from several sources and the ZAP was able to display them by alphabetical order or fill date. This patient was treated for COVID in February, treated for hypothyroidism and pain in May, treated for hypertension and reflux in July, and had been on medications for high cholesterol in the past. I didn’t see any blood thinning medications on the list.
Using this list, I could tell that she had filled all of the prescriptions she was prescribed in the last year and had not been treated for blood clots during that time. With this in mind, I started the patient on a direct oral anticoagulant (DOAC) and she was admitted to the hospital. Family members were not available to confirm her medical history and prescriptions until the next day.
Although the ZAP is often used for care transitions, annual visits, specialty consultation, and post-ED and hospitalization follow-up, the ability to rapidly obtain an accurate and up-to-date medication list shows that the ZAP can also provide immediate value for unscheduled care like ED and Urgent Care appointments. Without this access to Zus data, I would not have been able to make an informed decision on anticoagulation treatment in the ED, and this could have delayed her care until her family or previous care team could confirm her medication history. With PEs, I like to initiate treatment as soon as possible, and the ZAP provided information in real time so that my patient’s care could be tailored to her needs without delay.
Note: Certain facts have been changed to protect patient privacy.
Featured photo by Ian Taylor on Unsplash.
Dr. John Dayton practices Emergency Medicine with Intermountain Health and Stanford Health Care. He is the first Medical Innovation Fellow with Stanford’s Department of Emergency Medicine where he also completed a Biodesign Faculty Fellowship. Dr. Dayton is interested in digital health, AI, entrepreneurship, and medical devices. John is involved with medical innovation as a VC investor, as an advisory board member for NODE.health and AngelMD, and as a physician advisor for Zus on healthcare data interoperability and the physician user experience.

