In the first installment of the Zus Q&A series, we sat down with our resident healthcare data whisperer, Dave Boerner, to get his thoughts on the landscape of interoperability today. We laughed, we cried, and we told scary stories around the camp FHIR.
Tell us a little bit about yourself. Why should we care about your thoughts on healthcare data?
I’ve got 15+ years of health IT experience including:
- GE Healthcare IMLP
- Galen Healthcare, where I focused on integrations with AllScripts
- Orion Health, where I worked on the sales engineering team selling integration engines
- PatientsKnowBest, a PHR startup in the UK where I led solution architecture and enabled >2M patients to access their records
- Particle Health, where I helped lead the company go from 0 to 1 through series A
- Unqork, where I led sales engineering for healthcare and learned how to build solutions in a no-code environment
- Zus, my current role where I lead solutions design across pre-sales and customer implementation
I’ve done a lot around interoperability both from an implementation and GTM angle so my perspectives have been molded to reflect that. Integration in general is a very dry topic and slow-moving space, so many folks (understandably) don’t have the patience to stick to the field for long periods of time and really develop a nuanced understanding.
You like to talk about how healthcare data interoperability should value evolution as much as revolution. Say more.
Revolution is a lot sexier, because it introduces massive changes and has the potential to completely disrupt the current paradigm. And I love revolution. But interoperability, by definition, only works when you get to the critical mass of adoption. Even if a group has created the most revolutionary method for exchanging data, it won’t amount to anything if it isn’t widely embraced and implemented. That’s why FHIR is something I’m so excited about – it has actually hit widespread adoption. Healthcare is a huge beast of an industry and it moves forward incrementally, as opposed to leaps and bounds (at least interoperability-wise). What’s important, and what actually does make a difference, is to make sure that those incremental changes are in the right direction. So evolution, while not as exciting as revolution, is something we should still appreciate.
What do you think has been the biggest innovation in healthcare data interoperability of the past decade?
I’ll say 2 things: first, large scale FHIR adoption. This is important because the industry has finally embraced something beyond HL7v2. v2 is centered upon event-based messaging and keeping systems in sync, whereas FHIR allows you to pull any information you want and tell a story. Imagine that we’re sitting around a campfhir and I’m telling you a scary story about a ghost haunting. A v2-style story be as follows: “Bobby was born on July 5 2002, Bobby was admitted to the ER, Bobby had bloodwork done, Bobby’s results showed presence of blood cancer, Bobby died on May 2, 2015”. In comparison, the FHIR story would read, “Bobby died from cancer at 13 years of age”. Storytelling is much better when you don’t have to go event-by-event.
FHIR bridged the gap that v3 failed at. By nature, the FHIR standard makes it easier to share information between systems without requiring an event to happen, and because most everyone is using this standard, systems can communicate with each other in a universal medium. It makes the goal of HL7 v3 implementable.
Second: legislation in the U.S. is actually bearing fruit. You have the CURES Act, anti-information blocking, TEFCA, Sequoia Project, setting up these exchanges, most notably Carequality and CommonWell, to allow the exchange of healthcare data for treatment purposes. Think about the way that the industry has evolved: 20 to 25 years ago, almost everything was on paper and there was no sharing between systems. Meaningful use set up digitization of hospitals and created EMRs, which kicked off early data sharing.
Let’s think about this in terms of building a national transportation infrastructure: with the initial EMRs, we were able to build streets within towns that connected the grocery store to the gas station to people’s homes. Next came the HIE craze 10 years ago – this was like building highways between cities within the same state. The newest exchanges are nationwide, and so we have built the interstates across the entire country.
Right now you can only drive on these interstates with a treating provider, because Treatment Purpose of Use is what systems currently respond to, but in the (hopefully) near-term, Individual Access and other purposes should see an uptick in responses, which will open up a host of exciting use cases.
That’s not to say there aren’t exciting use cases in the Treatment space. With these exchanges, we are already traveling between states for uses like virtual consultations, and since I love analogies, that’s basically supercharging the interstates. It’s the Autobahn of interoperability.
Why is healthcare data interoperability important for healthcare providers?
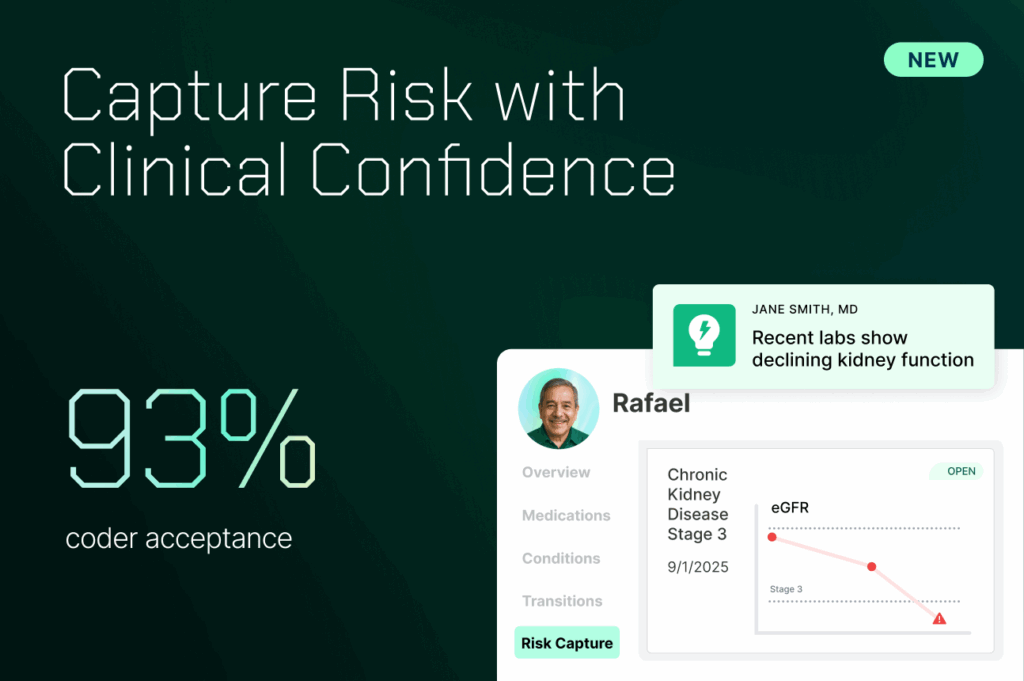
From a practical purpose, value-based care is getting lots of traction, and the goal there is to improve outcomes and decrease costs because providers and payers are entering risk sharing agreements. How do you do that? By reducing redundant tests, by increasing access to information about patients you wouldn’t normally have, and implementing novel strategies to treat patients based on this data.
This work unlocks revenue increases as well, such as increasing throughput, which allows you to spend less time asking patients questions and reviewing charts…which then empowers you to treat more patients and to deliver them better care.
In your opinion, why is Zus’s data offering exciting?
Because we turn data into information. We’re actually making it usable. The exchanges facilitated the sharing of data, but that didn’t make it usable. If you think about the experience the major EHRs have using these exchanges, their “external care” solution typically constitutes a clinical document tree with potentially hundreds of documents of C-CDAs, which are essentially as good as getting nothing. It’s not usable at the point of care. What Zus has done is actually take those documents and map them into information based around the FHIR standard, which our customers can consume in multiple experiences (API, Zus UI, EHR partnerships) and in multiple workflows (streamlined reconciliation process, full ingestion, etc.).
What’s your biggest takeaway from ViVE 2023?
- Nashville is so much better than Vegas.
- I’m good on fried chicken sandwiches for the year.
But in all seriousness, ViVE is my favorite conference on the circuit. Lots of innovative companies looking to disrupt the industry with new paradigms. I always think of these startups as building a car: that’s their value proposition. For those cars to run they need fuel, or in this case, data/information. That’s our value proposition. It leads to tons of fascinating conversations about what we can do to actually affect meaningful change in lives.
You’ve been referred to as “the bad boy of digital health.” Do you care to comment?
No comment.